Joe’s view: interoperability is the new black
- 15 June 2015
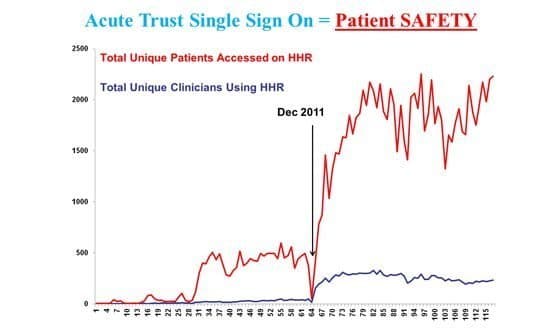
Can you tell when they switched on single sign-on for the Hampshire Health Record? Can you see when everything got a bit safer for the patient? Can you see the revolution?
Southampton signs on
In an exciting couple of months I have had three very interesting days in the interoperability area.
Firstly, Amir Mehrkar, the chief clinical information officer of the Hampshire Health Record, showed this slide during a recent CCIO Network site visit to Southampton. I think it is the most important slide I have seen in the eight years I have spent in the health IT arena.
Amir’s presentation showed how the Hampshire Health Record contains a rich portfolio of information about the patient, brought together from a variety of acute and primary care sources, using technology from Graphnet.
The idea is to improve decision making and patient safety by enabling clinicians in a variety of settings to access this information – and to let social care get a look-in, too.
However, what this slide clearly demonstrates is the importance to busy clinicians of single sign-on – fast access to that information. Smart cards and additional log-ins are a barrier to the use of integrated digital care records. The smart card has got to go.
The other triumph of the Hampshire Health Record is its common sense approach to information governance. If you are contemplating a local record sharing arrangement in your ‘regional interoperability community’ (and I know many of you are) then you could do worse than pay a visit to Southampton.
Amir also showed figures suggesting that when clinicians view the Hampshire Health Record inpatient stays are shorter. The business case writes itself.
I left Southampton a worried man, though. I had a growing sense of unease about my own practice. Clearly a shared record was making a difference in Hampshire; and I was aware that in my clinic I was blind to the content of the primary care record.
SystmOne reaches out
My second day out was as keynote speaker at the SystmOne National User Group. At a vibrant meeting, there were hundreds of SystmOne users comparing notes and suggesting improvements to its developer, TPP.
The SystmOne philosophy – “one patient one record” – is appealing on the basis that if an entire health economy buys into SystmOne the boundary between the primary care record and the secondary care record simply vanishes.
The problem, of course, is that the NHS is unlikely to want to put all its system supply eggs in one basket.
However, at SNUG interoperability was the hottest topic and the agreement between TPP and rival GP (and increasingly community and mental health provider) EMIS to collaborate on information sharing was the talk of the town. The nation expects.
This second visit convinced me that I must have a view of the primary care record from my clinic. It is starting to feel negligent not to have a view.
However, the Hampshire Health Record and SystmOne both took years to develop. I need a view into the primary care record NOW. How can I quickly get the view I need?
Flying the MIG
In my trust, we arranged a demonstration of the Medical Interoperability Gateway as deployed in Cumbria. I was staggered at the detail of information that can be viewed in a couple of clicks.
An elegantly simple consent screen – do you have permission to view, ‘yes’ , ‘no’ , ‘break glass’ and you are in. Works with EMIS, TPP et al so most of the country could use it.
A real-time view from secondary care into the rich detail of the primary care record. Some readers may recall that sometimes patients die for want of this kind of information
The ‘view only’ iteration of the MIG is reasonably priced and I feel the safety advantages make the business case compelling. Healthcare Gateway, the provider of the MIG, makes no bones about how it will make more money.
It can provide a ‘cost per message’ messaging system between primary and secondary care. I suspect this might end up as something of a blank cheque, so it’s not something I would consider switching on currently; a simple ‘read only’ view will do for now.
To get this view, I will need my current system supplier to amend my home screen to include a MIG viewer button to take me seamlessly into the primary care record. A paradigm shift in patient safety. A must have.
Why would a secondary care CCIO buy an electronic patient record that wouldn’t do this? What GP system supplier wouldn’t want to see this great leap forward in patient safety?
NPfIT2 without all that NPfIT stuff
If we were going to do NPfIT2, we wouldn’t be building any new systems. The GP record systems are already pretty damned good and are supported by vibrant user groups who continue to drive their continuous improvement.
Maybe, if we were doing NPfIT2 we would spend the taxpayers’ health IT pound on the infrastructure to join up existing systems and to provide real time messaging between systems. Maybe on an open source basis so that no blank cheque is required.
In a previous information revolution (1837), Rowland Hill wrote a report on the disjointed, expensive, insecure and multiple postal systems in the UK which led to widespread support for the development of the Royal Mail.
The problem it ran into was how to fund the network required to deliver mail nationally. Hill hit on the idea of the pre-paid postage stamp; “a small square of paper with a glutinous substance on the back”.
He open sourced the design through a competition that drew 2,600 entries. The winner was the Penny Black. Sales went from 70 million to 350 million in ten years. Maybe, if we are writing a blank cheque it should be to the NHS or an NHS Open Source Software Foundation.
Can you feel it? A number of factors appear to be aligning. Caldicott 2 with the “duty to share”, new models of care which blur the boundary between primary and secondary care, the willingness of companies like TPP and EMIS to cooperate, the Hampshire IG model and the rise of the open source community all suggest that the future is bright, the future is interoperable.


Joe McDonald
Joe McDonald is a practising NHS consultant psychiatrist. Over the past five years he has been an NHS trust medical director and national clinical lead for IT at NHS Connecting for Health – a stint that included 18 months as medical director of the Lorenzo delivery team!
His experiences in the National Programme for IT in the NHS have left him with a passion for usability and "end user knowledge networks.” He is the founding chairman of the National Mental Health Informatics Network. Motto: we don't get fooled again. Follow him on twitter @CompareSoftware




