EHI CCIO interview: Dr Phil Koczan
- 10 January 2012
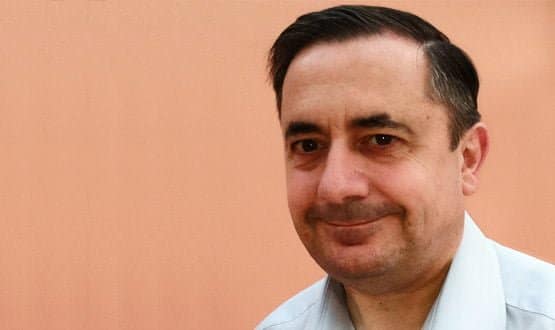
Dr Phil Koczan is the latest addition to the growing band of chief clinical information officers in the NHS.
He is the first with a role outside the hospital setting, and the first from a general practice background. His new role is as CCIO for UCL Partners, one of the five accredited academic health science centres in the UK.
It doesn’t run services, but instead exists to help the NHS in north central and north east London translate research and innovation into practice. His role is much more about informatics than energising IT implementations for clinicians.
Fascinated by IT
Dr Koczan has a long track record in general practice, IT and informatics. A GP for 18 years, he has also taken on various clinical advisory roles to Torex (which merged with iSoft in 2003), BT and the London Programme for IT.
“I have always had an interest in IT and computers,” he says. “In my early days as a GP I built my own computer and installed my own software.”
As a GP he was interested in how informatics can support better patient care – and in how barriers to sharing information can hinder it.
In April 2011, he became clinical director of informatics for NHS London, where he worked on a project that looked at bringing together clinical information from different healthcare settings for patients with chronic obstructive pulmonary disease.
This work led directly to his new appointment at UCL Partners, where he currently works one day a week but plans to expand to two or three days a week in the spring.
“We are still defining what we mean by CCIO,” he says. “Our thoughts are that it is about the information we need to share across the healthcare spectrum to support organisations to deliver good care right across the NHS.”
He lists the purposes for which information needs sharing: direct patient care; patient access to records; developing care pathways so that people with long term conditions can be managed effectively along a pathway; commissioning to provide information about what is actually being delivered and to what quality standards; research and transparency.
“In many cases this is the same data but different structures and rules are needed to deliver it,” he says. “The information governance is a very significant part of this agenda.”
Getting out of practices and trusts
Being embedded in UCL Partners will allow Dr Koczan to work across the entire health community as well as with partners in academia and R&D.
UCL Partners brings together several hospitals – for example University College London Hospital, the Royal Free, the London and Newham – as well as community providers, primary care and universities.
“What we find is that across London and within the partnership there are lots of examples of work going on, but it is all done in isolation,” he says.
“My role is very much about looking at what is happening; where and how do we move from small scale projects to large scale change.”
This work requires a clinician, he argues. “The reason you need a clinician, and specifically a chief clinical information officer, is that in many ways this is a translation role.
“You get technical people who design a technical solution that does not work clinically; you get clinical people who do not understand the technical constraints. That leads to lack of progress.
“I see my role as a translator to say ‘this is what clinicians need; this is what the technology can do’ and then work out how we move on.”
The work on data sharing in the COPD pathway is a good example, he says. It involved looking at how to join data from GP practices and secondary care records for patients with severe COPD.
It has enabled doctors to identify patients attending hospital who could be treated in the community, patients on the wrong medication, patients being over treated and highlighted patients who have never been diagnosed in primary care.
“We have found patients who are slipping through the GP net and that, for me, highlights the need for someone in a CCIO role who understands the technology and the clinical need.”
Moving beyond technology barriers
Dr Koczan says now is an exciting time to be in such a role. “Two or three years ago we could not have done the technology. Now it is doable.
“We have lots of technology around secure data warehousing, for example. The big question now is what we want to do with this technology and the data.”
Perhaps the biggest challenge is the information governance. “It’s one of those wicked questions where if you ask five people you get ten answers,” he jokes. “It’s a question of getting some shared understanding of what the governance rules are and how we address them.
“This is going to need a culture change among clinicians and patients to reach a shared understanding that we want to share data, can we do it safely and where do patient views and consent fit in.”
His appointment comes at a time when all of this is high on the policy agenda with the government demanding that patients have access to their own records and that the NHS deliver integrated care.
“I think it is a sea change that does help,” says Dr Koczan. “It may over simplify the problem and it may polarise views but it starts the discussions.
“In the past, we may have said ‘we want to do this’ and just been told ‘you can’t’. Now we need to do it and there is a policy driver to say ‘we have to solve this problem’.”
But with no “home” trust, how will he do his job? “You can never force these sorts of things on people,” he says.
“This is all about relationships and persuading people and convincing them that data sharing is a good idea, showing them areas where it is working, sharing the stories about where patients have benefitted, bringing them on board and continually pushing the message through.”
Exerting influence
One of the strengths of UCL Partners is that it already has the relationships and is set up to work through influence.
He does not yet know exactly where he will sit within the organisation but already works closely with the managing director Professor David Fish and chairman Sir Cyril Chandler.
“My vision is to try to make happen all the ideals that were embedded within the national programme,” he says. “This is where the national programme failed.
“It’s about engaging with clinicians and patients, and working together to solve problems. It’s about getting people enthused and working from the bottom up rather than telling them that this is what is going to happen to them.”