Expert view: Loukianos Gatzoulis
- 1 September 2010
 Loukianos Gatzoulis
Loukianos Gatzoulis
When we are ill, we suffer at home or at work. Symptoms can occur suddenly in the situations in which we need them the least. More often than not, there is no doctor or therapist available to offer immediate help or to check what is wrong.
Illness, in other words, can turn our lives upside down. But most of us tend to visit the doctor only on rare occasions, and often we wait until things go very wrong. Then we can end up being hospitalised.
Until now, there has been little alternative to this structure of care. Time and financial constraints limit the amount of attention that a healthcare system can offer to the ‘general’, non-hospitalised, patient.
The price paid by healthcare systems for this lack of attention is manifold. If deteriorating symptoms were recognised earlier in chronically ill patients, admissions to hospital could be avoided in many cases. If citizens at risk of a certain disease were monitored more closely, early intervention would be possible. And if patients were diagnosed more quickly, there would be less delay in starting treatment.
By offering personal health systems, ICT can help to resolve many of these issues. Broadly speaking, personal health systems are tools that bring care closer to the patient, tools that help to monitor a patient or person at medical risk.
Personal health systems make it possible to realise a less fragmented care process without a steep increase in the volume of care and without requiring the patient to visit medical facilities more often than before.
From diabetes to rheumatism: countless use cases
In chronically ill patients, for example, ICT tools can help to monitor all kinds of disease-relevant parameters. This includes weight monitoring and blood pressure monitoring in cardiovascular patients. Diabetic patients might use ICT to continuously document their blood sugar levels.
Psychiatric patients might use online tools that help care providers to assess whether the patient is on the verge of a relapse. Rheumatic patients might monitor their quality of life or pain levels digitally in order to make it easier to identify problems in everyday life. There are almost infinitely more examples of this kind.
But personal health systems are not only targeted at those who are already ill. Citizens at risk of a certain disease might also use ICT tools in order to detect the occurrence of a disease earlier. Personal health systems can also help to speed up diagnosis, since they allow symptoms to be documented when they occur and this information to be made available to the respective specialist.
There are two central issues that have to be addressed before personal health systems can become an integral part of healthcare in the future. One challenge is organisational: personal health systems have to be integrated into care in such a way that patients and healthcare professionals experience them as beneficiaries.
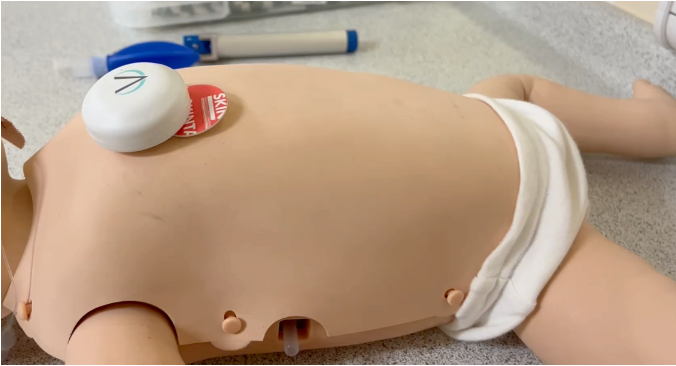
The other challenge is technical: it will be vital to design personal health systems to be both medically relevant and highly usable in the everyday life of patients. This is facilitated by increasingly smaller and more lightweight monitoring systems, and by ever more interactive and mobile documentation tools.
Under the umbrella of its Seventh Framework Program (FP7), the European Commission is backing research into PHS with the explicit goal of creating highly usable solutions that can be used at any time, worn while going about one’s daily business or at least carried around easily.
New projects which receive three years of EU funding from 2010 onwards deal with personal health systems in a variety of different settings and for patients with various different conditions, including patients with cardiovascular disease, suffering from depression, patients with cardiac implants, with stress-related disorders, diabetes, kidney diseases and psychiatric diseases.
Related links:
About the author: Loukianos Gatzoulis has a number of degrees in electrical and biomedial engineering and has worked in the wireless communication sector. In 2005, he joined the ICT for Health unit of the European Commission as a scientific officer. He is currently leading the research activities of ICT for Health in the area of personal health systems.
The views presented are those of the author and do not necessarily represent the official view of the European Commission on the subject.