Digital pathology: present and future
- 1 July 2010
 Pathology has never been the glamorous end of the health service and – unlike radiology – it has never formed a central part of the National Programme for IT in the NHS.
Pathology has never been the glamorous end of the health service and – unlike radiology – it has never formed a central part of the National Programme for IT in the NHS.
However, rapid developments in what the specialty can deliver and higher patient expectations have led to an increase in demand for pathology services over the past few decades.
“Lab medicine has matured massively in the last 20 to 30 years,” says George Philp, portfolio manager for pathology products at iSoft. “The 1970s and 1980s saw an explosion in what it could offer, with specialist tests being developed.
“In the 1990s and into the noughties, labs began to consolidate and centralise, partly in a bid to make themselves more efficient and partly as a response to a regulation and quality assurance regime aimed at improving standards.”
Consolidation and connectivity
Take the example of neonatal testing. The heel prick tests carried out on every newborn are now analysed in just 20 labs nationwide. Lincolnshire has consolidated its pathology services, as has Leeds and Bradford, creating a mega lab that deals with 3m specimens annually on behalf of three trusts.
More recently, pathology has begun to move out of the hospital and into primary care – or even into patient’s homes. “Anticoagulation and monitoring of Warfarin treatment is a good example,” says Philp.
Meanwhile, patients have started to demand tests. It’s no longer good enough for a GP to look in their eyes to check for anaemia, says Philp. Instead, GPs are ordering blood tests that are seen as non-invasive and safe. The patient feels as though something is being done.
All of this has translated into an explosion in the workload. “Labs are reporting year-on-year increases in their workload of 8 to 10 per cent,” says Philp.
So the question now facing pathology services is this: how can they deliver a high quality, safe service that is both efficient and responsive to change?
This question is at the heart of the ongoing review of pathology services that was set up in 2005 by the Department of Health and chaired by Lord Carter of Coles. Its second report was published late in 2009. It is still awaiting a DH response.
Among the second report’s 20 recommendations was that labs should continue to consolidate. From that stems another of its recommendations: pathology needs IT connectivity.
Contributing to the efficiency and quality agendas
That’s already a reality in some of the “mega labs” that are able to communicate across the multiple sites that they serve. The labs analysing neonatal heel prick tests recently notched up a world first when they started to send results to GP systems electronically.
But IT connectivity could go much further. “Laboratory management information systems used to be in a silo. To a large extent, they simply automated the process of producing a paper report in electronic format.
“Now they have to be able to send information to the hospital patient administration system, to cancer registries, to primary care systems and so on.
“Publication needs to be multi-faceted to many different places, using many different formats and structures. The NHS is driving standards on this and in an ideal world everybody would speak HL7 Version 3 with a Snomed dialogue. In reality, they don’t.”
A common language, if you like, would enable LIMS not only to report automatically in different formats and to different locations, but to become part of integrated care pathways, ending a pathway or starting a new one.
There are areas where IT can help pathology to deliver on the efficiency and safety agenda too. “Lab systems are incredibly data rich,” says Philp. “The challenge is turning data into intelligence.” Theoretically, LIMS could deliver early alerts on new strains of MRSA, say, or clusters of infections.
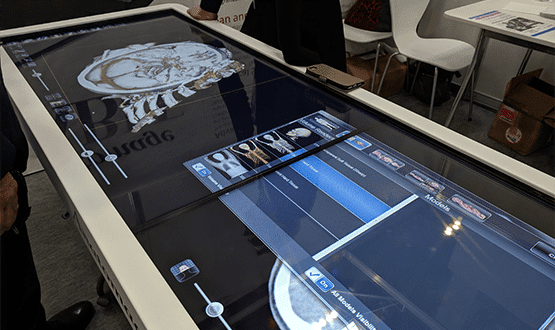
Digital pathology is another part of the piece. Where doctors can now view and share digital x-rays, the same could be delivered in pathology with digital images of slides.
The technology exists, Philp says, but so far it has not been implemented in full in the NHS. “The technology is there and the infrastructure. We can certainly hang on the coat tails of PACS and RIS in terms of where we store images, how we move them around and how we control access.”
Patient-centred services?
So while connectivity is important, there is a great deal more to pathology IT than connectivity. In 2008, the DH and NHS Connecting for Health published an information strategy for pathology and this too is about to be renewed.
Part of its vision was the creation of patient-centred services. Rick Jones, senior lecturer at the University of Leeds, was one of the leading lights behind it. He outlines what he would like to see.
“Pathology is in a supply chain,” he says. “Most of the contact with the patient is clinician contact and we sit behind the clinician.” In other words, doctors need information about which tests to do and what the results mean – but so, Jones argues, do patients.
Leeds and Bradford’s pathology department has made this information available on the internet. Doctors and patients can look up information tailored to their needs.
Pathology IT has a long way to go but some of the building blocks are in place. Standards for messaging are in place – though not adopted.
Business intelligence suites that will help pathology labs mine their information now exist. The infrastructure and learning from PACS/RICS could be adapted for digital pathology. Patient information is developing. Perhaps the next decade could see pathology IT coming of age.
Round table discussion on digital pathology, organised by E-Health Insider, sponsored by iSOFT.
E-Health Insider will be holding a round table discussion on digital pathology on 9 July 2010. At the event, sponsored by iSOFT, expert speakers including Philp and Jones will discuss current issues in digital pathology and future trends in this vital, but often unseen, area.
Questions that will be discussed include: How can digital pathology systems be used to streamline services further and make better use of NHS resources at a time of public spending restraint? What contribution can systems make to patient safety?
What can and should we demand from future systems? How are laboratory systems being adapted to the demand for integration of healthcare services? And where do patients fit?
However, EHI is interested in the views of readers on this subject. If you would like to make a comment or raise a question, use our comment functionality or email linda@e-health-media.com to help shape the debate.