Virtual wards: We are in danger of being eclipsed by our European neighbours
- 17 April 2024

There is huge scope to extend the reach and impact of virtual wards and remote monitoring. But the NHS must act now to make the best use of key developments, writes Tara Donnelly in the second of a two-part series
Great progress has been made in extending virtual wards across the NHS in England. It is leading the way on virtual ward provision. However, there is a risk of being eclipsed by other European countries on the use of remote monitoring for wider health care.
We can avoid this by focusing on five priority areas for digital home care going forward:
- Continue to grow our virtual ward provision – It is important to maintain the momentum on virtual wards and continue to grow services to reach more people.
- Increase tech-enablement – To realise their potential, and ensure they are truly equivalent to hospital care, all virtual wards need to be tech enabled. For more on this and virtual ward provision, see the first part in this series.
- Remote monitoring for emergency care – There are some innovative models that are highly copyable, interfacing directly into urgent and emergency care. We are seeing examples of Urgent Care Response teams being able to start remote monitoring locally, a great development which ought to be standard care. Teams in North Bristol NHS Trust are providing remote monitoring to selected patients from same day emergency care, such as those with cellulitis, obviating the need for admission. In Herts Urgent Care the GP rapid response vehicle is equipped with remote monitoring so that they are prepared to use this to prevent an admission. It would be fantastic to see this concept extended further and across ambulance trusts.
- Remote monitoring for elective recovery – We are starting to see remote monitoring easing the elective backlog, for example ensuring people are ready for major surgery and reducing last minute cancellations. Gloucester Hospitals NHS Foundation Trust is advancing this in orthopaedics, with a focus on hip and knee replacement. As well as getting waiting lists down, the internal business case for investment outlines the income to the trust from completing significantly more operations than without this digital prehab service.
- Beyond virtual wards into long term condition management – There are now some great examples of wider digital home care impacting on those living with long term conditions and achieving dramatic reductions in hospitalisation rates. Some of the best are the results being achieved in heart failure by the team at Imperial College Healthcare NHS Trust and the wider North West London population led by Carla Plymen. There is also impressive work in Airedale on chronic obstructive pulmonary disease (COPD) where they’ve reduced emergency admissions by up to 50% in their cohort of over 4,000 patients, and Frimley Health and Care ICB where they have focused on the highest risk and most deprived patients in their patch, supporting them with remote monitoring. In addition to reducing secondary care use, these sites have observed marked reductions in other aspects of NHS utilisation, including a 28% reduction in outpatient follow-up appointments within the cohort at Frimley and a halving of GP visits in Airedale.
Proactive care
COPD is the umbrella term for a group of progressive lung diseases including emphysema and is very much a disease of deprivation, as well as one of the most common reasons for an emergency admission and ambulance journeys. It is also highly seasonal, contributing disproportionately to winter pressures.
One of the most rewarding projects I’ve been involved in recently has been working with the terrific team in Bristol who are adopting a COPD hub model across the ICB, focusing on those at highest risk of admission. Those at the top of the pyramid are offered extra support, including remote monitoring, health coaching and signposting to services that can help them.
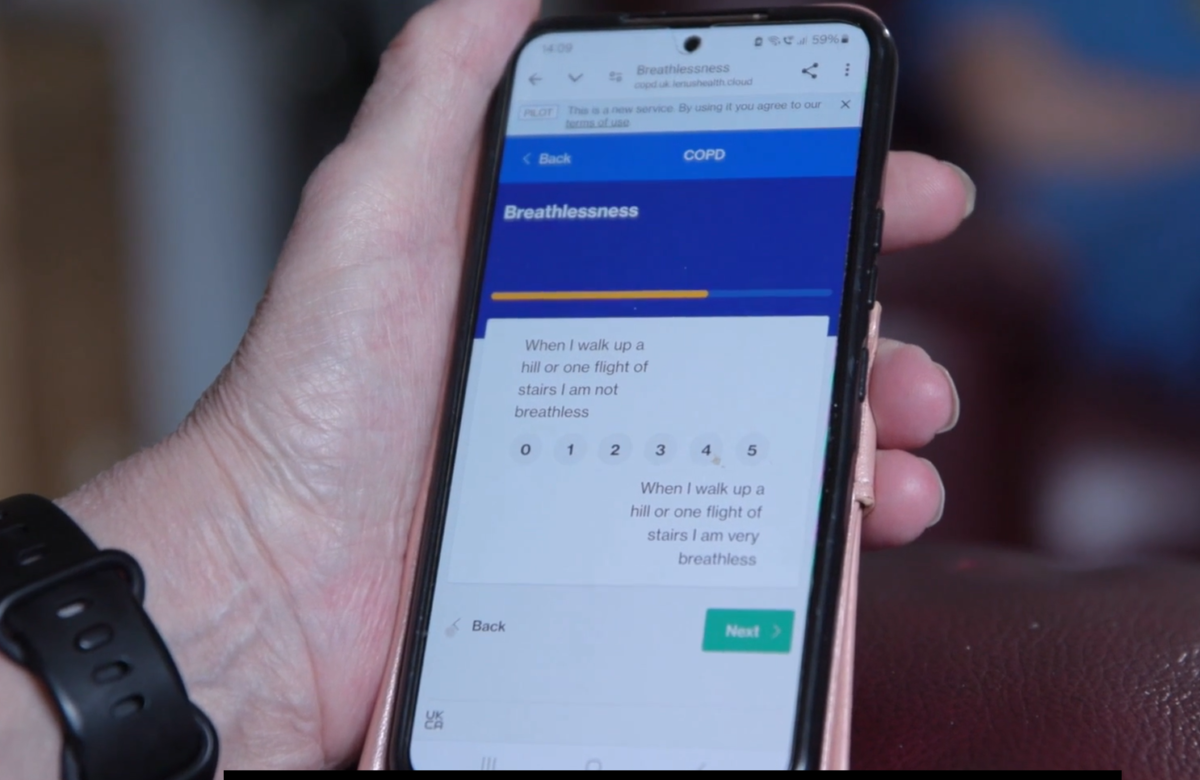
Patient enrolment began in January and 21% of those joining the programme are from the 10% most deprived group. It is a really impressive collaboration between all parts of the NHS in Bristol, North Somerset and South Gloucestershire, Sirona Care and Health and the tech partners involved, Doccla, who deliver clinical monitoring and the remote monitoring tech, and myMhealth who produce the companion app myCOPD.
The model being implemented across Bristol should be the future of effective long term condition management in the NHS, giving those with severe disease and highest risk of hospital admission extra help to keep them well and out of hospital.
Wider benefits
As well as providing improved care and support to COPD patients, there are much wider benefits too. By preventing admissions and catching deterioration early we are able to increase the resilience of the NHS to better meet the needs of other patients. The benefits may include rapid dispatch of an ambulance or speedy admission as an emergency. Lower hospital occupancy rates should also make the working lives of dedicated NHS clinicians much more pleasant and sustainable, meaning elective waiting times can be reduced, as bed availability is more predictable. Getting it right for this key cohort of patients means benefits for everyone.
Remote monitoring in Europe
In Denmark, they are providing remote monitoring to all those with severe COPD this year, so convinced is the Danish government of the benefits. I spoke this week to Ria Hoegh Kaffka, one of the architects of the initiative, who said: “It is so amazing that we are finally here, I am very proud of that”. It would be fantastic if this became the model of care in the NHS.
In France, they are extending remote monitoring to any patient where their doctor believes they would benefit. In Germany DiGA [regulation covering digital healthcare technologies] has recently been extended to encompass remote monitoring.
We can be rightly proud that the NHS in England has led the way on the expansion of virtual wards for people with an acute need to have that care provided at home. With vision, there is no reason this same technology can’t be used to keep those with long term conditions well and out of hospital, just as our European neighbours are doing.
Implications for the next government
I would love to see whoever wins the next general election making this commitment and helping transform not just the quality of health care but the effectiveness of how our health system works, with an emphasis on prevention and keeping people well, avoiding admissions rather than waiting for them to occur and then responding.
Without this commitment and transformation, I fear we will be eclipsed by the more proactive and innovative approaches of our European neighbours. And if this happens, we will struggle to recover the NHS.
 Tara Donnelly is the founder of Digital Care and former chief digital officer at NHSX/NHS England.
Tara Donnelly is the founder of Digital Care and former chief digital officer at NHSX/NHS England.
Read the first part in this series here.




2 Comments
I’m almost 62 and was diagnosed with COPD in 2006 I was extremely short of breath and constantly tired due to my Emphysema, I was introduced to Natural Herbs Centre and their COPD Ayurveda Protocol. I started on the COPD Treatment last year, my symptoms gradually diminished including my shortness of breath, wheezing and fatigue
Surley thats because your model for the Virtual Ward is so basic and limited.
Comments are closed.