General election 2024: Health leaders share their views on digital priorities
- 30 May 2024
Following the government announcement that a general election will be held on 4 July 2024, we asked health tech leaders and think tanks for their views on what the priorities should be for digital health. Here’s what they had to say:
Malte Gerhold, director of innovation and improvement at The Health Foundation
“Technology holds huge potential for improving care, raising productivity and empowering patients to manage their health – and the Health Foundation’s polling shows the public are, on balance, happy to see greater use of many types of technology in healthcare.
“But to capitalise on this potential, the NHS will need more than just new ‘kit’. We’ll only get the benefits from new technology if it’s implemented and used well – and that requires the right training, infrastructure and support too.
“NHS clinicians tell us the biggest barriers they face in using technologies effectively include access to IT expertise, poor connectivity and lack of implementation support, so the next government will have to sort these issues and fund ‘the change’, not just ‘the tech’.”
Hassan Chaudhury, expert in residence at the London Institute for Healthcare Engineering
“Investment into digital health without first resolving key workforce concerns is a false economy. We’re nothing without our people and we’re pushing most to burnout, with many leaving in the midst of a global health workforce shortfall.
“We must reduce pressure on the system, improve integrated working, improve prediction and early warning of deterioration, embed and extend timely population health interventions based on data, support citizens to self-care and decrease the friction that clinical teams face with technology. Otherwise it’s just throwing good money after bad.
“Tech for the sake of tech is of no use to anyone. We need a government that is brave and principled enough to not continually interfere, and to take the NHS out of its current status as a political football so it can manage it with technocrats.”
Tom Whicher, chief executive at DrDoctor
“The NHS is close to the crucial tipping point of tech adoption and Labour have an open door opportunity to accelerate this progress. They shouldn’t change too much.
“More money is needed but there are great foundations in place already in the NHS app and patient engagement platforms. If Labour doubles down in its commitment to this infrastructure and aggressively invests in products to deliver truly hybrid healthcare, positive change for clinical practice is within touching distance.
“Maximising data and a tactical investment in AI could be the gamechanger to improving back office productivity.
“Yes there are exciting clinical benefits such as analytics and cancer work which AI could support, and we should embrace that, but a pragmatic approach which uses data to stratify and prioritise patient journeys (both remotely and in person) will do away with the clunky ‘first in first out’ ways of working and ultimately help us to deliver better patient outcomes”.
Sam Shah, NHS consultant at Royal Wolverhampton NHS Trust
“The priorities for health tech need to be meaningful, realistic and affordable. They need to help solve some of the problems facing citizens and clinicians in the near-term future.
“First up, make patients’ lives easier by making it simpler when engaging with the NHS or any healthcare provider.
“Patient access to their records, irrespective of which provider has created the entry, through either an NHS application or any third party of their choosing; extend the concept of single patient sign on.
“Address the issue of booking appointments across the NHS and fully adopt a booking standard that makes it much easier for patients to book whether that’s across primary care or secondary care.
“For clinicians, we need to reduce the information overload but also make it much easier to see a comprehensive view of a patient’s history. This needs to be agnostic of software system but a data layer that does have some resemblance of a single source.
“The view of this data needs to be nuanced around the context of care. There needs to be a reality check on the national electronic patient record (EPR) strategy and some transparency around patient safety, followed by realistic investment in primary care, mental health and community – as well as the beast that is the acute sector.”
Sarah Woolnough, chief executive at The King’s Fund
“Despite sustained efforts, the NHS waiting list for elective care remains stubbornly high at 7.5 million.
“Long waits for care have been brought down before, but it takes time. It wasn’t until 2008 that the last Labour government got waiting times within the target. Clearing the backlog within five years would take real effort and focus and may mean other ambitions in health and care will be slower to realise.
“Addressing long waits for care will also need greater government focus on preventing ill health in the first place, and crucially, shifting more care outside of hospitals into the community so people’s conditions can be managed without the need for acute care.
“Labour’s commitment to increase the number of CT and MRI scanners is welcome, but it is less clear what action the party would take to achieve its goal of increased efficiency in the health service.”
Nick Wilson, chief executive at System C
“Whoever is in government from 5 July must prioritise the key aspects of digital health so critical in helping deliver a sustainable health and social care system.
“Both main parties have stated that supporting UK tech is a high priority. The most direct way of doing that is to ensure that the NHS and public sector prioritise the amazing innovation and talent in UK tech by buying British as a priority.
“While funding has never achieved the levels required to really drive improvements to the level we might like, many billions of pounds has been spent on tech over the past 20 years.
“So rather than changing out often perfectly good solutions on the promise that something shiny will miraculously solve all the problems, a new government should instead prioritise building on investments made to date rather than opting for rip and replace strategies.
“There is a golden opportunity to connect care with existing systems. A “one solution” for every care setting and different user type will cost billions and take decades.
“For most integrated care systems (ICSs) and organisations, they will never come close to delivering on the benefits promised to make the business case stack up. Connecting existing high-quality systems across ICSs where they exist, will deliver value (such as productivity savings), far more quickly and at far lower incremental costs compared to wholesale system replacements.
“Speed and accountability are critical. We must accelerate decision-making to meet digital maturity and productivity targets.
“Devolving decision-making and hence empowering ICSs, along with NHS trusts, is crucial to facilitating more regionally tailored and effective digital networks.
“The next government needs to ensure investment prioritises change and transformation as we all know that digital on its own cannot achieve digital maturity and deliver the benefits the system so desperately needs.”
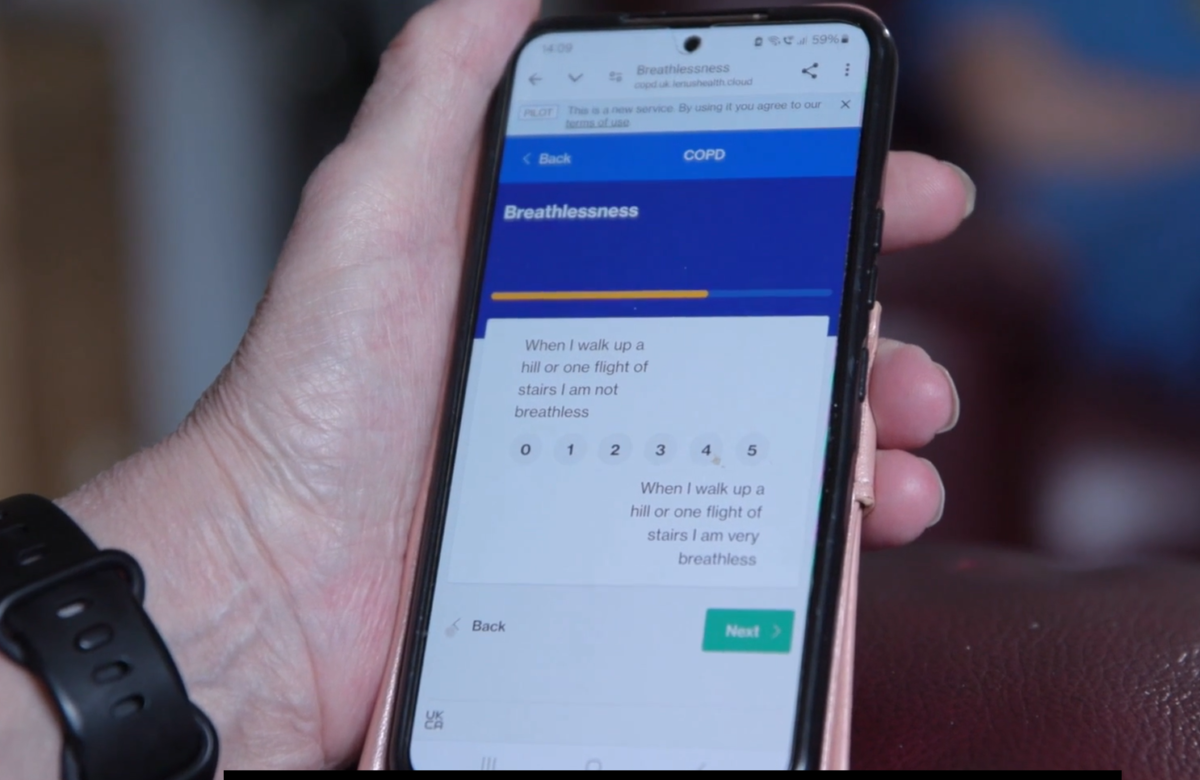
Jim McNair, director at Lenus Health
“The upcoming government’s digital health priorities should facilitate proactive management of major health conditions, emphasising early diagnosis, risk stratification and proactive care.
“This should include proactive identification of patients with undiagnosed disease, and diagnosis resource coordination across different healthcare settings using digital tools.
“Additionally, for diagnosed cohorts, risk stratification and proactive care should be based on structured healthcare data from across regional and place-based providers.
“To avoid unscheduled care, supported self-management can be achieved through digital tools, and population management strategies.
“With these approaches in place proactive AI can help identify and intervene with high-risk patients before their conditions worsen. Implementing these measures will alleviate pressure on hospitals and healthcare systems within the NHS, promoting a more proactive approach to maintaining the well-being of the UK’s ageing population in their homes.”
Carmelo Insalaco, chief executive at Rapid Health
“The next government should focus on maximising the efficiency of our current healthcare workforce. Simply increasing the number of doctors is not the answer, the priority should be on freeing up doctors’ time from unnecessary tasks and utilising technology to better manage and balance patient demand.
“Smarter technologies can transform and further elevate the modern general practice access model by providing a comprehensive understanding of demand and capacity in primary care.
“We need to streamline and better integrate patient pathways between primary and secondary care to meet the needs of local areas. This integrated approach is crucial for reducing the strain on hospitals, which is partly caused by pressures in primary care.
“By doing so, we can fully leverage smarter technologies, simplify patient care pathways, and maximise the efficiency of our current healthcare workforce. This will also help us identify the true gaps in the existing workforce.”
Julian Coe, managing director at X-on Health
“The announcement of the general election heralds a pivotal moment for the UK’s future, and this is particularly true in relation to primary care. With ever-increasing levels of demand and an increasingly ageing population, patients want access to primary care as a priority.
“However, on the flip side, there are challenges around funding, staffing, and GP access that have become increasingly visible and the government must prioritise the support and development of this essential service.
“Digital telephony plays a key part in the bigger picture enabling efficient appointment scheduling, reducing waiting times and increasing patient satisfaction, but to improve access the government must encourage the adoption of technology with relevant training to support the workforce and to help signpost patients to the correct services.
“Primary care is the front door to the health service, if it is not fully supported then these challenges will continue to impact the health and wellbeing of the population.”