Rewired 2024: Funding pledge provokes opportunities and challenges
- 15 March 2024

Recent investment in NHS IT is a vote of confidence in digital leaders but brings with it complex questions about digitisation and its impact, speakers argued during a keynote session at Digital Health Rewired 2024.
Last week’s Spring budget included a pledge to put £3.4bn into NHS IT, an investment NHS England’s interim transformation director said was a doubling in funding.
Vin Diwaker said it was “significant” investment that constitutes an expression of confidence in those working in healthcare digitisation.
While Matthew Taylor, chief executive of membership body the NHS Confederation, praised the work of NHS England in securing the money from Treasury, he said it should be placed in context.
“It’s a promise made by someone who actually doesn’t have to deliver on it [given the likelihood of a change in government at the next election], and we don’t know what the baseline is – so it’s £3.4bn on top of what?”
Productive questions
The funding pledge is tied to a government aim to improve productivity across the public sector. Diwaker clearly stated that drive “was one of the key reasons we got investment”.
But the reality is that vendors and users alike have long struggled to confidently prove that the likes of EPRs, for example, lead to efficiency savings. That is not least because of the time involved in their implementation.
Daniel Johnston, clinical workflow specialist at Imprivata as well as an emergency nurse, said his experiences had led him to “appreciate how hard it is to stand up IT both within a department, a service, and not least regionally and nationally”.
It is also hard to measure the impact of digitisation on efficiency, a point acknowledged by Diwaker. “NHS England need to develop a framework over the next year about how we measure productivity which actually makes sense to the way you experience the delivery of services and makes sense to politicians.
“The worst thing we could do is to come back to this event in four years’ time and say: ‘Look at all these programmes, all these products we’ve put in, all the stuff we’ve delivered, and actually still not be able to have evidence of the benefits.”
“Wonky triangle”
The aim will be for any productivity improvements delivered by health IT investment to sit alongside related improvements in patient care.
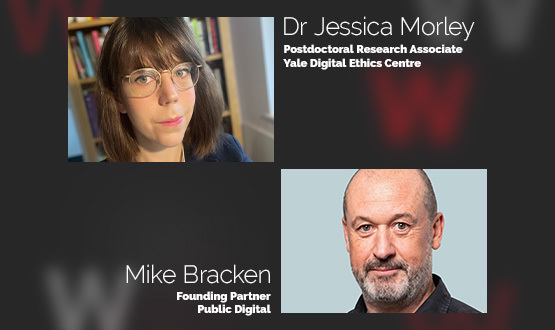
But in a barnstorming presentation which drew a rapturous audience response, Jessica Morley – postdoctoral research associate at Yale University’s Digital Ethics Center (DEC) – contended that simply was not possible.
“[It’s said that it’s possible] to simultaneously improve population health, experience of care, and reduce per capita cost. I say that is nonsense – I don’t think you can achieve those things at once; I think what you can achieve is a wonky triangle.”
She said there was also important questions to be asked about precisely how any investment is used.
“There is a very big difference between could and should when it comes to digital transformation in regard to healthcare. Most of the time when we’re in these rooms what we talk about is ‘could’ – could I do it, is it technically feasible, have we got the infrastructure?
“My point is that it’s not just about technically feasible, it’s also about whether can be ethically justified.”
Morley argued data-related laws are no longer fit for purpose in an increasingly digitised world of healthcare, particularly with AI developing at speed.
And she characterised governance of digital healthcare as “woefully outdated”, rooted in a world in which healthcare interventions were centred on one-to-one interactions as opposed to broader population health work.