From Pain Points to Pain Relief – user-centricity in health innovation
- 9 March 2023

Ahead of Digital Health Rewired 2023, Digital Health strategist and CCIO Advisory Panel member Dr Lia Ali discusses how bringing user-centricity into health innovation could bring us closer to better health for all in a quick, safe and efficient manner.
In my first year of medical practice in an acute hospital I was involved in the care of a woman who had a rare condition causing paralysis of her body from the neck down. She had multiple complex needs from specialist medication to surgical intervention, physiotherapy to tube feeding, hoist transfer to pressure area management.
She was desperate to get home.
Our team’s care of her involved understanding her experience through history taking, observation, assessment, management and reassessment. We needed to identify every pain point on her route home and come up with ways to address each one.
Understanding a person’s experience is fundamental to any successful healthcare intervention including those that are technology enabled. Design-led approaches can be used in a similar way to clinical methods to understand user experience and achieve complex problem solving as well as considering how best to deliver solutions. When this is done well it allows the value of an intervention to be realised quickly, safely and efficiently.
The value of user centred design approaches is well documented in and out of healthcare. McKinsey tracked the design practices of 300 publicly listed companies over 5 years. Companies with strong design practices (as measured by the McKinsey Design Index) increased their revenues and shareholder returns at nearly twice the rate of their industry counterparts.
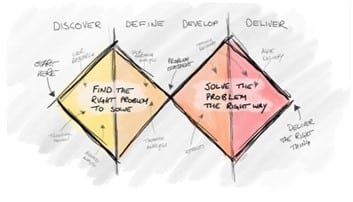
Tero Vaananen, Head of Design in the NHS Transformation Directorate at NHS England, encourages us to see that user centred design is the strategy to ‘find the right problem to solve and to solve the problem the right way’ (Vaananen, n.d.). It allows us to delineate between products and services so that ‘services achieve outcomes that solve problems for users’.
Solving problems effectively requires the right problem framing and the ability to surface user needs rather than wants. It also means we, as those writing policy or developing, buying and implementing technologies, need to be aware that we are not our user.
Good UCD practice encourages a non-hierarchical approach to design. Listening to the loudest, most powerful voice in the room doesn’t mean that the right thing for people will get built.
I have come up against this many times when trying to explore how a truly holistic healthcare system can be designed when the legacy systems are all geared towards the needs of the bricks and mortar, acute, physical health hospital.
Problem framing, user research, service design, prototyping and iteration are some of the many areas will touch on during our session titled ‘Integrated Care Pathway Transformation’ at Rewired on the Integrated Care Stage at 3.15pm on March 14.
Tony Browne, head of innovation and design in the Digital Care Models Team in NHS Transformation Directorate, will give us the benefit of his extensive experience of design led digital transformation for whole countries and global companies and how he is bringing that knowledge and expertise to the NHS.
Tony will give us an overview of the theories and frameworks that are at the heart of design thinking and user-centred design in a way that can all understand the practical and potential immediate benefits to the system, patients and staff.
Erica White, associate director of innovation at Royal Free London NHS Foundation Trust, will share how their team have applied user-centric methodology to great effect, for example in the Lantern system and the Midwife Safety App.
Finally Sarah Amani, chief nursing information officer at Dorset HealthCare University NHS Foundation Trust will join us to inspire us with how she is beginning the journey of embedding user centricity in the system she works in.
We can’t afford to wait to get started with this approach. In too many areas of health and social care people’s experiences are getting worse not better. The health inequality divide must not widen.
Join us next week as we want to hear how you are doing this and how we can move this forward as a community committed to improving health outcomes.
‘The cure for the pain is in the pain’
Rumi