Winners of Summer Schools NHS Hack Day aim to replace MIG
- 24 July 2018
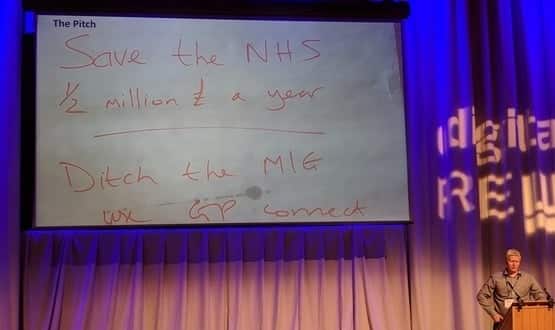
The winning project at the Summer Schools NHS Hack Day demonstrated how a tool for accessing GP records can be replaced with a free NHS alternative, potentially saving half a million pounds a year in just one region.
The NHS Hack Day, run as part of the Digital Health Summer Schools, was the first ever to be run mid-week to enable NHS teams to more easily participate. Over 100 people took part, including teams from NHS trusts and companies big and small.
Projects that had been developed by teams over the two days of Hack Day were then demonstrated live to hundreds of NHS IT leaders attending the Summer Schools, who then voted in a live online poll.
‘Done-ocracy’ narrowly beat ‘NHS Choices on Call: tackling digital inclusion’ in a knife-edge vote. NHS Choices on Call used APIs to take NHS Choices data and use Amazon AWS voice services to make Choices data voice searchable, enabling easier access for people who are not digital natives.
For ‘Done-ocracy’, the name a play on the Hack Day ethos of creating a ‘do-ocracy’, the team managed to replace the Medical Interoperability Gateway (MIG) with GP Connect, potentially saving the NHS millions. MIG is currently widely used across the NHS to enable records to be shared.
Over just two days, a team of developers from Northumbria Tyne and Wear NHS Foundation Trust (NTW) worked with colleagues from other trusts, NHS England and members of the NHS Digital Spine Team, to show how GP Connect could be used to replace the MIG for the sharing of GP records.
MIG is currently widely used to provide access to GP records in the North East, but the proprietary system – owned by Healthcare Gateway, a joint venture between GP system providers EMIS and INPS – costs the local region half a million pounds every year.
“We wanted to see whether NHS Digital’s GP Connect service could be used instead,” explained Darren McKenna, CIO at NTW.
“In just two days of focused effort, by bringing the right people together, we were able to achieve more than we could have done in many months. It’s really an amazing achievement.”
McKenna said the team planned to continue developing the GP Connect interface into a tested, production-ready version able to replace the MIG locally, and share this with all other parts of the NHS that want to use it.
“If we can do this it will mean that not only will we be able to save half a million a year in the North East, but other parts of the health service will be able to make similar savings,” said McKenna.
One of the visitors to the Summer Schools was Dr Simon Eccles, NHS CCIO, who after his keynote speech took time to visit the Hack Day and speak to teams taking part.
Dr Marcus Baw, organiser of the Summer Schools NHS Hack Day, said: “For me, it felt like the best one we’ve ever done in terms of real life NHS IT outputs, live APIs, engagement from NHS trusts and start-ups.”
In 2017, the first Summer Schools NHS Hack Day was run the weekend immediately following the Summer Schools, and while a success, participants said the four-day commitment required was too much to ask. So, for 2018 the event was moved to mid-week for the first time.
Dr Baw commented: “The sharing ethos and electric atmosphere was just like previous NHS Hack Days and so I don’t think we’ve lost anything in the transition to weekday events.”




4 Comments
I still stand by original to this. To run this stuff locally costs money, and rather than this being in licensing, support fees, and chargeable implementation, the cost is full salaries, training, pensions, hosting, development, fixing, information governance, clinical safety, implementation, support, etc that goes into running a professional and reliable service. I’m just saying the building your own thing is not sun shine and rainbows and I challenge that saving that was hastily scrawled on a presentation. Sure, companies are making a profit on delivering services to the NHS, but that means there are businesses able to continue investing in talent, hardware, competitive pricing etc. It’s hard to build this tech, and even harder to implement it. When you don’t need a trainer, or an engineer, etc anymore you just stop paying for the service. When it’s your staff, that means redundancies. Another cost.
I think its an excellent achievement and an example of why its important to revist the view that many organisations have on putting in place a development team.
Done correctly the cost can beat third parties and this is an example of how that can be achieved. Of course there is a running cost but no where near the level expressed by The Insider….
As I understand it the major development was already done by NHS Digital to create GP Connect as a service and this is an alternative to the commercial MIG. A number of areas have been keen to make use of GP Connect now it is available. The beauty of what was done at the Hack Day was to demonstrate/set up a way to link GP Connect to a local service, with the commitment that how that was done will be made available to others. So more of a local implementation of an interface rather than a product in the sense you are describing I think.
It’s a great move… but I’d like to see the financial analysis on how much it will cost to hire developers (or pay the team’s salaries), develop the product, maintain, host, implement, and support such solutions within a health economy. A team of 20 people (across dev, implementation, management, support) on a salary of £50k each (lets make that an average across junior and senior talent) is £1 million, and that’s without taking the other elements of running this kind of service into account. That’s also without including other employer fees. So, it’s fine to save £500k to give to a supplier, but then you have to take on the costs that supplier already took a hit for to develop, implement, and maintain that service. It’s exciting, however, to see what can be done when smart people come together under one roof. I’m wary though of home-brew systems returning that eventually need replacing because the appetite for the running costs runs out.
Comments are closed.