Laura’s digital disruptors: even better than the real thing

“It fools your mind. Once you use it, you just forget you’re in the lab doing it; it feels like you’re in the theatre.”
So declares Rob Middleton, professor of orthopaedics and head of Bournemouth University’s Orthopaedic Research Institute, which recently installed facilities for specialist virtual reality training.
With its powerful immersive technology, virtual reality has the potential to allow medics to train and practice numerous times in a simulated environment. It not only benefits healthcare workers, but also provides innovative treatments for patients suffering from mental health issues.
Surgical training in the future
The institute has become a global leader in virtual reality training. Offering the world’s first virtual reality arthroscopy, it is also the first centre in Europe to offer a virtual reality training system for a total knee replacement.
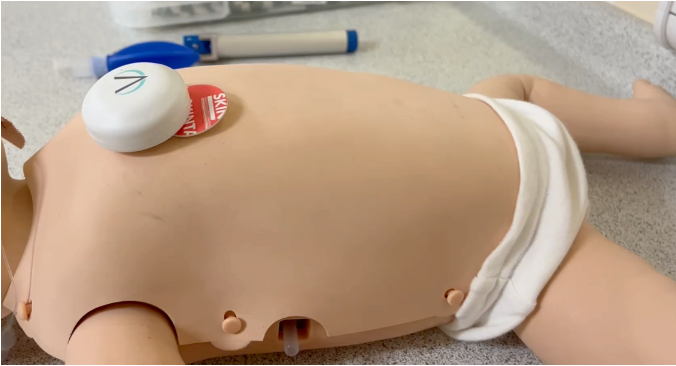
Middleton says the offering is about answering the question, “how do we train our surgeons for the future?” Traditionally surgeons learn on the basis of “see one, do one, teach one”, but with a limited number of training opportunities, and access to cadavers pricey, this offers an alternative.
The orthopaedic departments at the nearby Poole and Bournemouth district hospitals have been or are coming in the next month, with 20 to 40 surgeons expected to play with the new technology free of charge.
Middleton also suggests a future with personalised virtual reality – the day before the operation, he says, consultants could scan the patient, and then practice on the simulation.
95% akin to real life
So advanced is the virtual reality that Middleton describes it as “95% of what it’s like to actually do the operation”, in contrast to simulations, which he puts at 30-35%.
By recreating the environment with the lights, noise, clothes and people of the operating theatre, the stressful realities can be replicated and encountered before seeing an actual patient.
The institute partnered with Swiss company, VirtaMed, to develop the virtual reality trainer, and the software is open source. Middleton also wants to pair up with the university’s renowned animation school, hoping that the department can develop the training further.
Crossing national borders
A Dutch start-up, MDLinking, has an international outlook on how virtual reality can help doctors. It connects medics across the globe and has 360 degree virtual reality videos of routine operations that can be watched on YouTube (warning: blood and cuts).
Gijs van Acker, a surgeon at the Dutch Medisch Centrum Haaglanden hospital who films the videos, says the footage may have even more worth in developing countries.
“Here we have a lot of hospitals, with lots of possibilities for young doctors to join a procedure, but in Africa or South America, there are lots of countries where you do not have that coverage.”
In these locations, “they skipped the whole desktop era, they jumped immediately to wi-fi”, van Acker adds. So if virtual reality or instructional videos can be used: “I think that’s a huge step to change the world and improve global healthcare”.
To date there are four videos, with another two in the pipeline for an appendicitis and caesarean section. There would be more, but there is a lengthy post production process, as a doctor has to sit next to a video editor to clarify which frames are valuable.
“Huge potential” in mental health treatment
While still in its infancy, there have been successful trials for virtual reality being used as a treatment. A Medical Research Council-funded study at the University of Oxford was a small and short term trial into how the technology can treat persecutory delusions.
The results, published in the British Journal of Psychiatry, found that the 30 mental health patients from Oxford Health NHS Foundation Trust benefitted from just 30 minutes of immersion in virtual reality.
Daniel Freeman, a professor of clinical psychology at the university who led the trial, says that virtual reality has a “huge potential” to reshape mental health treatment and its delivery.
Patients experienced different potentially stressful situations, such as a crowded tube or lift. Half the group tackled their fear through exposure, which involves putting people in the situation they are afraid of. The other half used a cognitive approach where the patients dropped their defences to see how the other people would react.
Freeman said the latter approach which “derived from a good understanding of paranoia, had really large effects over and above those of the other approach”. As psychological issues are so bound up in the environment, he adds, this technology could be used for a whole range of mental health problems.
“What’s great about virtual reality is that the learning transfer to the real and also people are much more willing to try different things in virtual reality because they know it’s not real.”
Engaging potential patients
The technology can also be used to let the public into the often closed off world of surgery. The Imperial College Centre for Engagement and Simulation Science (ICCESS), which is located at Chelsea and Westminster Hospital NHS Foundation Trust, has engaging the public as part of its remit.
Fernando Bello, one of the co-leaders of ICCESS, says that people of all ages are invariably attracted to virtual reality. “They find it fascinating, both in terms of technology but also in terms of its implications”.
Engaging the public has mutual benefits: “We find that it extremely powerful to allow the public to relate to medicine and surgery in a different way. But equally, from the other side of things, it also allows clinicians and technologists to better understand the perspectives of the public and their anxieties.”
He points out that another application for the technology, although it is not yet routine by any means, would be to allow the patient to come in an experience their operation, to see what the surgery will be like.
Virtual reality will not become reality
However, Bello stresses that while virtual reality has huge potential, it won’t ever replace real-world experience.
“The way we see it, and the whole the trend at the moment, is to use this technology to make sure that trainees get certain competency levels in terms of understanding the procedure, the operation, the examination before they actually faced with having to do it on a patient,” he says.
About the author: Laura Stevens joined Digital Health News in summer 2016 and covers the ‘digital patient’ beat – covering the latest in mobile, online, apps, start-ups, and disruptive technologies of all kinds. Follow her @DH_LauraStevens