Sutton integrates social care and health record
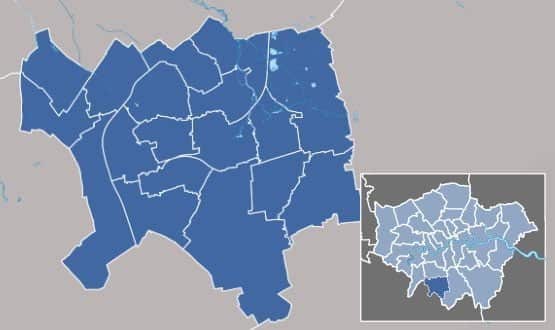
The London Borough of Sutton and NHS Sutton Clinical Commissioning Group have created a shared care record with social services involvement from the outset.
The council and the commissioning group gained finance from the Integrated Digital Care Technology Fund – or tech fund 2 – for the Sutton Integrated Digital Care Record, which is built using Graphnet’s CareCentric.
The project went live in December, sharing GP and social care data with Epsom and St Helier University Hospitals NHS Trust, but is already being rolled out more widely.
Siân Hopkinson, director of performance and primary care, told Digital Health News the rapid pace of the project had been helped by neighbouring Kingston having a similar project, using the same technology.
“That is definitely something that other areas should consider,” she said. “It’s very rare that someone has a completely new idea. So if there is something you can look at, beg, borrow or steal, then do it. It’s much easier than starting with a blank sheet.”
One of the things that Sutton hoped to borrow from Kingston was its information sharing agreement but Hopkinson said this had rewritten to take account of local concerns.
The involvement of the council also raised consent issues. The council has rewritten its paperwork, so that new clients are asked for their explicit consent for their data to be included in the record.
Existing clients are also being asked for explicit consent, but some user groups, such as those with learning disabilities, present particular challenges.
Despite this, the SIDCR holds data from local GP and social care records, pulling data from the council’s Framework-i, which is supplied by Servelec-Corelogic.
The information is being shared with A&E staff from Epsom and St Helier hospitals, which has just integrated access to the record into its own electronic patient record.
Hopkinson said single sign-on to both systems was critical for success. “It means staff can access it [the SIDCR] from inside their clinical system, and they won’t even know they are looking at another record. They just see GP and social care data.”
The project is working on similar single sign-on access for community and out-of-hours staff, who use Adastra. And it is planning to include further data feeds from the hospital, which will focus on discharge information, and from mental health services.
The latter was not in scope for the tech fund 2 bid, and is the subject of another bid for funds from the Government’s ‘transformation’ pot; but Hopkinson said GPs were keen to have access to mental health records.
Unusually, the project has also commissioned independent research into the impact of the shared record; which had to show a return on investment over ten years to qualify for tech fund money.
It has developed a baseline questionnaire to determine how much time staff spend collecting the information the shared record contains; and has discovered that staff in A&E spend around 100 hours per week collecting information on patients from GPs.
“When you think that those practices are also taking calls, and finding information, and faxing or passing it over; then the productivity savings should be considerable,” Hopkinson pointed out.
The project is also going out and pro-actively collecting stories about using the record. “We had T shirts printed to promote the record,” Hopkinson said. “I went into A&E wearing one myself, and a junior doctor came up and told me he did not know how he had done his job before he had the information in front of him. Having people say things like that makes all the effort worth it.”
Graphnet’s CareCentric underpins the Kingston Health Passport and is also used for record sharing in Hampshire, Berkshire and Manchester. Its chief executive Brian Waters said Sutton’s benefits programme was “detailed and particularly impressive” and its results would be shared with its user base.



