Driving innovation in Detroit
- 23 January 2013

Detroit is best known as the home of the US car industry, enjoying a remarkable resurgence after being written off just a few years ago.
A similarly spectacular turn-around has been achieved by one of the US city’s biggest healthcare providers; underpinned by embracing electronic patient records and innovation.
Lisa Gulker, director of innovation at Vanguard Health, a network of eight hospitals in Detroit, says she become a nursing informatics leader almost by accident after the organisation decided it had to digitise to survive a decade ago.
“Detroit Medical Centre was in dire financial position in 2004-5,” she says. “It wanted to use quality of care as a differentiator and to use electronic medical records as a driver of improved care.”
Taking a step forward
Gulker says she was volunteered for her role by her boss: “She told me that there was a project called EMR that was a six month project. After that, she said ‘you can go back to regular duties’. I looked at the scope and my director said ‘you already said yes’.”
Gulker, who spoke at the first CCIO Leaders Network Annual Conference at EHI Live 2012, says there is a lot to recommend this way of getting involved in IT projects and, eventually, becoming a chief clinical information officer.
“If you don’t have role or title yet, don’t worry. It will come as you move to an electronic world; there has to be clinical leadership on practice,” she told the event.
The original Detroit project was to do all eight hospitals in less than two years, digitising them almost from scratch. “We were completely paper based apart from results. It was a big bang at each site,” Gulker explains.
Vanguard now runs a single Cerner Millennium system. It has reached HIMSS Level 6 and is getting close to stage 7 [the HIMSS levels are a measure of the maturity of a hospital’s adoption of EMRs, run by the US Healthcare Information and Management Systems Society – and 7 is as high as they go].
“That’s eight hospitals and eight cultures,” jokes Gulker. “We did a shake the whole institution to the core – very few people think that change is good most other people see as a problem.”
Sorting out the scope
Gulker says Detroit was able to achieve so much because “clinical leaders decided on the scope and ownership from the very beginning.”
She adds that her CCIO-equivalent role was essential for three reasons. “To provide clinical ownership, engagement and empathy – the three top three things to bring to this role.”
She said that the empathy needed is not the touchy feely kind. “It’s mostly ownership for patient care and practice.”
“As clinicians we have a personal connection to meaningful work,” she further explains. “Empathy is about acknowledging that real world experience and human connection.”
But for this to happen there must be a clear imperative from the top of an organisation embarking on this kind of project.
“At Detroit Medical Centre, it was a clinical project from the start – only the brightest and best clinicians were picked to lead the project.”
Driving clinical transformation
The focus at Detroit and across Vanguard has been to use the EMR as a tool to help drive clinical transformation.
“We committed to one standard of care: to use the same order sets across our hospitals, the same nursing documentation and sets of tools.”
Elements of this ownership included strong organisation structures, such as clinical councils accountable for standards and workflows.
These included the most senior clinicians in the organisation. “We have strong clinical oversight that has to approve any changes based on evidence in literature and best practice.”
As a result, the hospital group now uses one single patient record database and is starting to have a life-long record.
“We call informatics clinical transformation,” says Gulker. “We are most concerned with how our system is a clinical tool.”
As such, she is concerned to make sure that the system delivers measurable benefits, for instance around patient safety.
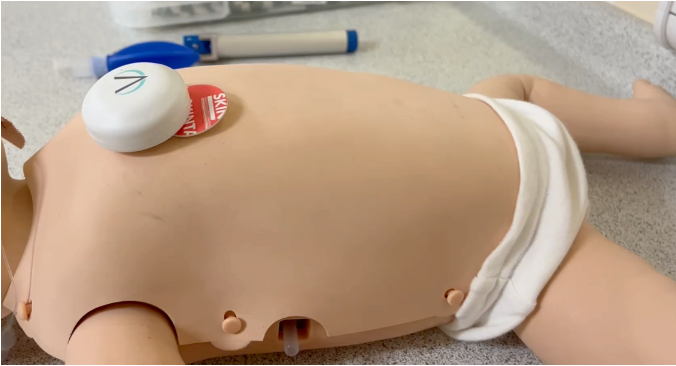
At the conference, she told how she delayed Detroit’s go-live of a neonatal barcode project until the supplier could supply the 3D barcodes needed for neonate babies; something it had said was impossible as the wrist bands were too small.
“I said I don’t want to go live with barcode neonate meds administration until we can get the technology solution we need. That’s the kind of ownership and leadership this role takes. So we said no and the IT people scrambled to make it work.”
You need a good partnership with suppliers “but don’t expect them to solve all your problems or bet between the clinician and the patient,” she added.
Have an idea, win an award
The chief executive at Detroit committed one million dollars a year to ‘EMR Awards’– a user suggestions programme in which best project gets funded to the tune of $250,000 a quarter. “If something about the EMR is bugging you, you submit your idea,” Gulker says.
She adds that the ‘EMR Awards’ are a great way to keep clinicians engaged after project go-live. The initiative has received 869 ideas, completed 112, and selected 129. The majority are major practice issues. As part of the initiative, Detroit also posts details of progress reports.
“I’ve been as Detroit for 21 years and this is the most exciting work ever done in my career,” Gulker concludes.